 |
| MLE homepage | Research | Medical Physics | UCL |
|
Photoacoustic imaging Images of tissue-mimicking phantoms | References | Contact
The technique relies upon irradiating the tissue with nanosecond pulses of low energy laser light. At near infrared wavelengths, due to the relative optical transparency of tissue, the light penetrates deeply (several cm). It is also strongly scattered. This results in a relatively large volume of the tissue becoming "bathed" in diffuse light. Through the processes of optical absorption and thermoelastic expansion, broadband (~30MHz) ultrasonic acoustic waves are excited throughout the irradiated volume and propagate to the surface. Here, as in conventional pulse-echo ultrasound, they can be detected using an array of ultrasound detectors and spatially resolved to provide a 3D image of the internal tissue structure. Penetration depths of several cm have been demonstrated using near infrared (NIR) excitation wavelengths with sub-mm spatial resolution. For shorter penetration depths of a few mm, higher resolutions of approximately 50µm are achievable. A key advantage is that the discriminatory mechanism is based upon the strong optical contrast of different tissue types offering the prospect of identifying anatomical features that are indistinguishable using other radiological modalities such as ultrasound or X rays. For example, haemoglobin (and its various oxygenated states) provides strong optical contrast at NIR and visible wavelengths making the technique well suited to imaging blood vessels – by comparison, the contrast of conventional ultrasound images tends to be limited by the relatively poor echogenicity of blood vessels. In addition to the direct visualisation of blood vessels the high contrast offered by haemoglobin provides the opportunity to indirectly detect abnormalities such as cancerous lesions that are accompanied by characteristic changes in the surrounding vasculature through angiogenesis. Additional advantages of the technique are that as a non-ionising method it avoids the safety concerns associated with X-ray imaging and has the potential to be configured as a relatively inexpensive portable instrument for bedside use or screening purposes. To advance the technique towards clinical application, a programme of research comprising the development of a forward model of photoacoustic signal generation, image reconstruction methods, wideband high sensitivity ultrasound receivers and related instrumentation is underway. Photoacoustic images in tissue-mimicking phantoms Laboratory experiments in simple “blood vessel” tissue phantoms have been carried out to assess potential penetration depth, axial spatial resolution and contrast [10]. For evaluation purposes, these experiments were carried out in the so-called forward photoacoustic imaging mode in which the detection of the photoacoustic signals and delivery of the excitation laser pulses take place on opposite sides of the target. For most clinical applications it would be necessary to position the detector on the same side of the target that the laser pulses are delivered to - termed backward mode imaging [8]. However for the purposes of evaluating the concept in the first instance, the forward mode provides a convenient and essentially equivalent configuration.
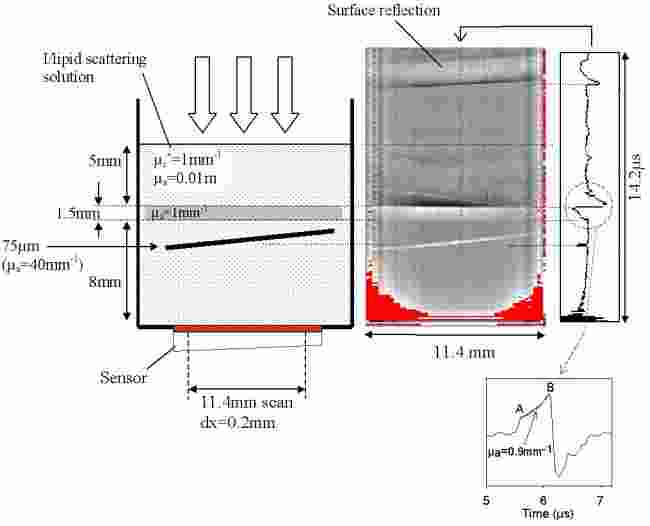
Figure 2 Forward-mode photoacoustic depth profiling of plastic absorbers in a scattering liquid (Intralipid: µs’=1mm-1 and µa=0.01mm-1). The optical properties of the Intralipid scattering solution were chosen to be approximately representative of "background" tissues such breast tissue in the NIR. The absorption coefficient (µa=1mm-1) of the 1.5mm thick absorber is comparable to that of blood in the NIR. The waveform on the right represents a profile through the centre of the image. The "surface reflection" is the reflection of the photoacoustic signal generated in the 1.5mm absorber from the surface of the Intralipid. It appears at an angle because the water bath was slightly tilted. On the far right is an expanded view of a signal (taken at a different point) generated in the 1.5mm thick absorber. By fitting an exponential between A and B, a value of µa=0.9mm-1 (in good agreement with known value of 1mm-1) was obtained thus illustrating the quantitative nature of this type of imaging. Incident laser fluence: 0.02 J/cm2, pulse duration: 7ns [10]. Figure 2 shows the set-up and depth profiling images of a 2 layer tissue phantom. Nanosecond optical pulses from a frequency doubled Q switched Nd:YAG laser were passed through a negative lens to expand the beam to a diameter of 1cm and directed on to the surface of the phantom. This resulted in an incident surface fluence of 0.02J/cm2 - well within the maximum permitted exposure (MPE) level for nanosecond pulsed laser irradiation in the NIR incident on skin. The photoacoustic signals were detected by the sensor head at the bottom of the water bath – for more on the sensor array [8, 9, 10] and related instrumentation click here. Briefly however, the sensor is a Fabry Perot interferometer illuminated by a large diameter laser beam. Acoustically induced changed in the optical thickness of the interferometer produce a corresponding change in its reflectivity. By scanning a photodiode along a line across the beam reflected by the interferometer, a line array of ultrasound receivers is effectively synthesised. At each point of the scan, the detected time-dependent photoacoustic waveform was averaged over 100 shots and captured. The set of signals for the entire line scan were then linearly mapped to a greyscale and displayed as shown in figure 2. No further processing or image enhancement was performed. Figure 2 shows that the signals from both plastic absorbers can be clearly identified. The thickness and depth profile of the 1.5mm absorber are obtained by spatially resolving the time-varying signals (using the speed of sound in the absorber and the Intralipid respectively) at each point along the scan and then back projecting vertically along the line-of-sight at each detection position. The thickness and position of the 1.5mm absorber obtained from the image in this way are in good agreement with the known values. Whilst this approach is valid for the 1.5mm absorber which lies parallel to the detection plane, care needs to be exercised in similarly identifying the position of the 75µm absorber. This is because it lies at an angle to the detection plane. The acoustic signal at each point along the scan therefore emanates not from a point vertically above it but one that is offset to the left. For such situations, where the photoacoustic source geometries are of large lateral extent and therefore emit near-planar waves, a far-field receive beamforming approach would be required for accurate reconstruction of the image. When applied to tissue imaging however, where the lateral source dimensions are generally much smaller and the wavefronts non-planar, it is a near field synthetic receive focussing or equivalently radial back projection approach that is generally required. Whilst the results in figure 2 clearly demonstrate the ability of this approach to localising regions of enhanced absorption in turbid media, a greater penetration depth than 5mm would be useful for biomedical tissue imaging. The above experiment was therefore repeated but with an increased Intralipid layer so that the 1.5mm absorber was now 10mm below the surface of the Intralipid. The beam diameter on the surface was reduced to 6mm thus increasing the fluence to 0.05J/cm2 but still within the MPE. In all other respects the experimental procedure was identical. Figure 3 shows that the absorbers can still be clearly identified to a depth of 10mm.
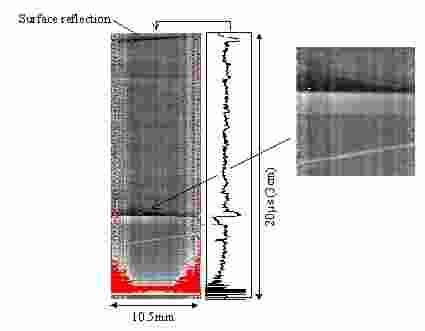
Figure 3 Image shows results obtained using an identical arrangement to that depicted in figure 2 but with an increase from 5mm to 10mm in the thickness of the Intralipid layer (µs’=1mm-1 and µa=0.01mm-1) above the 1.5mm plastic absorber (µa=1mm-1). Incident laser fluence: 0.05 J/cm2, pulse duration: 7ns [10]. |
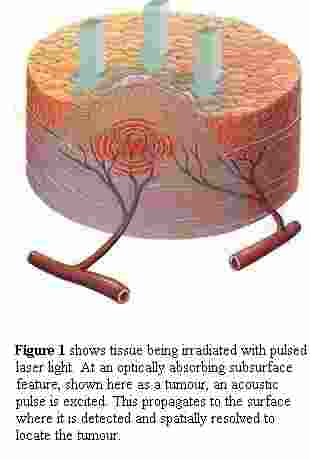 A key area of research for the group is the investigation of a
new broadly applicable method of non-invasive medical imaging, based upon
the photoacoustic effect, for visualising the internal structure and
function of soft tissues. Applications including imaging the breast for
the diagnosis and screening of cancer, the assessment of vascular disease
[
A key area of research for the group is the investigation of a
new broadly applicable method of non-invasive medical imaging, based upon
the photoacoustic effect, for visualising the internal structure and
function of soft tissues. Applications including imaging the breast for
the diagnosis and screening of cancer, the assessment of vascular disease
[